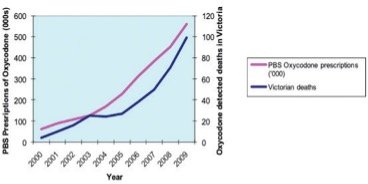
Whilst opioids are amongst the most necessary and widely prescribed classes of drugs to treat pain arising from tissue trauma and surgery, in the last five years Australia has seen a dramatic rise in the incidence and amount of opioids prescribed. This has resulted in parallel increases in prescription opioid associated mortality (death) and morbidity (harm).
A typical patient harmed by consumption of prescription opioids is not characterised by an individual seeking medication through deception and doctor shopping. The patient harmed by prescribed opioids is often aged 30-40, male, a blue-collar worker taking their medication in accordance with their health provider’s instructions.
Table 1 – Prescription Opioid Mortality
| Respiratory Depression |
| Accidental Overdose |
| Interactions with other medication and alcohol |
| Addiction and tolerance |
| Mental health and behavioural disorders |
| Motor vehicle Accidents |
| Emergency department visits and unplanned hospital admissions |
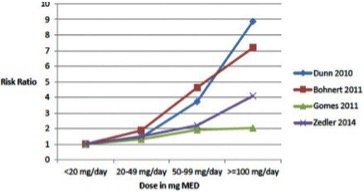
Addiction to opioids can occur after as little as six weeks of treatment, and in amounts in excess of 40 milligrams of morphine equivalent (MME)/day the risk to benefit ratio increases exponentially. Injured workers commenced upon opioids to manage their pain have an increased incidence of permanent impairment and never returning to work.
Table 2 – Factors that have contributed to the rise in opioid prescription:
| Wrongful acceptance of peer reviewed literature that concluded tolerance and addiction to opioids when prescribed for non-malignant conditions is rare |
| Widespread promotion and marketing of opioid treatment for non-malignant pain by pharmaceutical companies |
| Increase in number of medications with opioid side effects |
| Increased expectation of short stay surgery and pain free surgery |
| Increased waiting list times for public health services for chronically painful conditions |
| Lack of opioid education for patients and healthcare providers |
| “consumerism over professionalism”. The effect of healthcare consumer pressure for pain relief influencing professional advice and prescribing habits. |
As the harms inherent in recent opioid prescribing practices have achieved greater public awareness, there have been a number of initiatives introduced by health care institutions, professional associations, state and federal authorities (include Coronial recommendations), to adopt measures to prevent further escalation of this problem.
Table 3 – Regulatory responses to the opioid crisis.
| Introduction of real time monitoring of dispensed prescriptions |
| Up classification of weaker opioids in the poisons register |
| Introduction of smaller pack sizes of opioids |
| Improved warning labels on medication packs for side effects and interactions with other substances |
| Narrowing of TGA prescribing indications for opioids particularly sustained release preparations of opioids |
Opioid prescribers now find themselves between a rock and a hard place whereby they face professional sanction if they are seen to over prescribe opioids and yet can paradoxically face common law sanction if they prescribe too conservatively and cause harm through failing to adequately treat an individual’s pain.
Opioid Stewardship is a recently coined term to describe a set of coordinated interventions by healthcare providers to improve and evaluate the safer use of opioids to protect patients. Opioid stewardship initiatives have shown us that the majority of patients do not need to use the entire quantity of medications they are dispensed and that unused opioids are frequently held in reserve for future use either by the individual or their family and friends.
Table 4 – Opioid stewardship
| Better education of patients about interactions between opioids and other consumed substances |
| Improved coordination of prescribing between healthcare providers |
| Close monitoring of patient’s opioid consumption (often by telephone) |
| A plan to de-escalate and cease opioids after a given period of time |
| Patient recall and review if pain not adequately improved or decreasing |