Vaginal and uterine prolapse is a common gynaecological issue that requires surgical repair in about 30% of women. The aggravating factors are childbirth (prolapse of the vaginal walls and the uterus is a common problem affecting more than 40% of women following childbirth), family history, chronic pressure in the pelvis from constipation and chronic cough. The condition often runs in families and becomes more symptomatic with aging requiring surgical correction.
Traditional surgery used a technique similar to darning and led to frequent recurrence and the need for additional repair procedures.
Synthetic mesh (woven polypropylene non absorbable suture material) that had been used for several decades in repairing hernias, initially appeared to be a dramatic improvement for assisting in treating pelvic organ prolapse in women. While many women had an excellent and ongoing positive outcome with repair of pelvic organ prolapse with polypropylene mesh, others suffered unexpected complications that include:
- Exposure of mesh through the vaginal skin,
- Erosion of mesh into bladder, bowel or pelvis,
- Infection, exposure and discharge from exposed areas of mesh,
- Distortion of the pelvic tissue leading to chronic pelvic pain,
- Nerve damage.
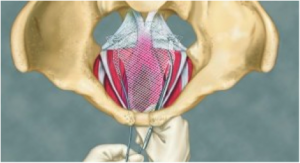
These complications have been attributed to the mesh material itself – rather than the surgical procedure. There is evidence to suggest that with time the mesh itself contracts causing distortion and additional tissue scarring. Evidence suggests that the size and weight and amount of the mesh are relevant.
Ongoing assessment of women suffering from mesh related complication requires expert pelvic floor assessment by a specialist gynaecologist to assess for residual mesh related damage. The surgery to remove the mesh is difficult and can often lead to additional damage to surrounding structures including nerves, blood vessel, bladder and bowel.
This article was written by Dr Philip Hall, Gynaecologist